Background: The prognosis for patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) is poor, even if treated with salvage chemotherapy and autologous stem cell transplantation. CAR T cell therapy provides long-term remission in only 40% of patients. Epcoritamab, a subcutaneous CD3xCD20 bispecific antibody developed using the DuoBody ® platform, received accelerated FDA approval for adults with R/R DLBCL not otherwise specified, including DLBCL arising from indolent lymphoma, and high-grade B-cell lymphoma after ≥2 lines of systemic therapy. Single-agent epcoritamab has demonstrated deep and durable responses (overall response rate, 63%; complete responses, 40%) and a manageable safety profile in patients with R/R large B-cell lymphoma in the EPCORE NHL-1 trial (Karimi et al, ASCO 2023, abstract 7525). Combining epcoritamab with antineoplastic agents that have different mechanisms of action may offer enhanced clinical benefit to patients. Therefore, EPCORE NHL-5 (NCT05283720) evaluated the safety, tolerability, and preliminary efficacy of epcoritamab, as well as defining its recommended dose when coadministered with other antineoplastic agents in patients with non-Hodgkin lymphoma. Here, we present results from arm 1 that evaluated epcoritamab combined with lenalidomide in patients with R/R DLBCL.
Methods: EPCORE NHL-5 is a phase 1b/2, nonrandomized, open-label, multicenter study. In arm 1, adults with CD20 + R/R DLBCL (ECOG 0-2) received subcutaneous epcoritamab (weekly during cycle 1-3, every 4 weeks during cycle 4-12) and oral lenalidomide (once daily on days 1-21) for 12 cycles of 28 days. Patients had received at least 1 prior combined systemic therapy that contained an anti-CD20 monoclonal antibody. The primary endpoint was the identification of dose-limiting toxicities (DLTs). Key secondary endpoints included investigator-assessed best overall response by Lugano 2014 criteria and time to response. Safety endpoints included severity and incidence of adverse events (AEs) including AEs of special interest to epcoritamab (cytokine release syndrome [CRS], immune cell-associated neurotoxicity syndrome [ICANS], and clinical tumor lysis syndrome).
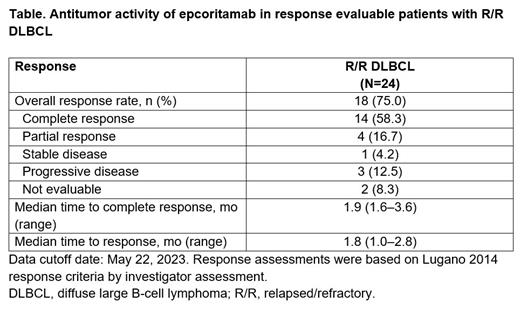
Results: As of May 22, 2023, 26 patients (median age, 71 years; DLBCL, n=24 [92%]; follicular lymphoma grade [G] 3b, n=2 [8%]) had received epcoritamab plus lenalidomide. Median duration of epcoritamab exposure was 3.8 months (range, 0-7.5) and median duration of lenalidomide exposure was 4.0 months (range, 0.1-8.2); 15 patients (58%) remain on epcoritamab and lenalidomide. Median number of prior lines of therapy was 1 (range, 1-4), with 15 (58%) receiving 1 prior line of anticancer therapy. Six patients (23%) had received prior CAR T and 2 patients had undergone hematopoietic stem cell transplantation. One DLT (neutropenia) was observed. The most common G3-4 treatment-emergent AEs (TEAEs) were neutropenia (n=15; 58%), anemia (n=4; 15%), thrombocytopenia (n=4; 15%), and febrile neutropenia (n=3; 12%). Primary granulocyte colony-stimulating factor prophylaxis was not mandatory. TEAEs led to epcoritamab discontinuation in 1 patient (3.8%; thrombocytopenia). No patients experienced a TEAE leading to death that was considered related to epcoritamab. CRS was predominantly low grade (73% [19/26] any grade; 65% G1-2; 8% G3) and occurred mostly after the first full dose (C1D15). Preliminary biomarker analysis showed pharmacodynamic profiles consistent with the mechanism of action of epcoritamab. These include predictable cytokine peaks immediately after the first full dose (IFN-gamma, IL-2, and IL-6) with a rapid and sustained depletion of peripheral B cells. One patient experienced ICANS (G3), which resolved after 2 days. Among response-evaluable patients (n=24), the overall response rate was 75% (95% CI, 53.3, 90.2). Complete metabolic responses were seen in 14 patients (58%) and partial responses in 4 patients (17%), of which 3 were ongoing at time of data cutoff ( Table). Median time to first response was 1.8 months (range, 1.0-2.8). Follow-up is ongoing.
Conclusions: Epcoritamab combined with lenalidomide showed promising antitumor activity with a tolerable safety profile in patients with R/R DLBCL.
Disclosures
Avivi Mazza:AbbVie: Honoraria. Kim:Sanofi: Research Funding; Boryung: Research Funding; Roche: Research Funding; Kyowa-Kirin: Research Funding; Beigene: Research Funding; Donga: Research Funding. Grande:AbbVie: Other: Advisory Board. Lavie:AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Advisory Board and Travel/Accommodation expenses; Medisson: Honoraria, Membership on an entity's Board of Directors or advisory committees; MSD: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel/Accommodation expenses, lecture; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Lecture; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Lecture; Roche: Honoraria, Other: Advisory Board. Chism:Regeneron: Other: Advisory Board; AstraZeneca: Other: Advisory Board. Seliem:AbbVie: Current Employment. Jeng:AbbVie: Current Employment. Joshi:AbbVie: Current Employment. Siddani:AbbVie: Current Employment. Assaily:AbbVie: Current Employment. Sacchi:Genmab: Current Employment. Dinh:AbbVie: Current Employment. Avigdor:Novartis: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees, Other: Travel/Accommodations/Expenses; Gilead: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; MSD: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal